“Before all of this, I always pushed having a positive attitude. It’s a frustrating disease, but I’ve got to look forward and improve every day.”
On June 16, 2019, John Soisson woke up with a bad headache. He couldn’t get out of bed. He fell, tried to get up, and fell again.
He couldn’t talk. The left side of his face was drooping. Jeanne, his wife, called 911.
Paramedics arrived and rushed John to Fisher-Titus Medical Center, a Level III Trauma Center in Norwalk where surgical specialists provide comprehensive care to patients with traumatic injuries.
Results of a CT scan and MRI showed evidence of a massive stroke and extensive tissue damage.
Doctors decided to transfer John to MetroHealth Medical Center, a Level I Adult Trauma Center and Comprehensive Stroke Center 60 miles away. Because dense fog was grounding all medical helicopters, a Fisher-Titus nurse rode in a local ambulance with John to manage his IV medication. The nurse happened to be the wife of a Norwalk firefighter who worked for John, the city’s Fire Chief.
New tests at MetroHealth confirmed an acute right middle cerebral artery stroke. A large blood clot in the cerebral artery was preventing blood from getting to the brain.
Because John wasn’t a candidate for tPA, a clot buster medication, or a thrombectomy, a mechanical procedure to remove a blood clot from an artery or vein, he was placed under close supervision in MetroHealth’s Neurocritical Care Unit (NCCU). There, doctors and nurses managed his fever, blood glucose, blood pressure, and body temperature. They conducted neurologic exams and evaluated function at the bedside.
After five days, John was moved to the MetroHealth Rehabilitation Institute. He began working with occupational therapist Heidi Rost, and physical therapist Jennifer Nagy. He also had speech and music therapies.
Slowly John regained strength and movement on his dominant left side. His mild cognition impairment and swallowing improved.
Stepdaughter Leah Schaffner, a trained physical therapist, practiced walking with John in the evenings. By the time he wrapped up six weeks of therapy, John was walking without any assistive devices. Still, someone always stayed close by, just in case.
“For John, that was his big milestone. And to witness his progress was really cool,” Leah said.
Another milestone was when John passed the modified barium swallow study test on the fourth try. That day was a celebration, said daughter Lindsey Esker. “He was just so over it,” she said. “It was a huge moment for us.” John finally could get a Sprite that wasn’t thickened.
Waiting for John at home was a fire truck, two ladder engines and the 17 men from the Norwalk Fire Department.
The next day, John started outpatient therapy with Lisa Garber (PT), Liz Galvin (OT) and a speech therapist.
Liz Galvin said John’s incredible work ethic wasn’t a total surprise, given the organizational skills needed to excel in his chosen career. “When he came to his appointments, he had an agenda.”
John needed to work on a lot of things affected by the stroke: one-sided neglect (visually not paying attention to anything happening on the left side of his body and to his left), coordination, dexterity and using his dominant left hand for tasks like brushing his teeth, shaving, eating, and writing.
After a couple of weeks, John had made significant progress with motor function in his left hand and arm. His coordination, dexterity and grip strength had improved. He was managing his daily self-care with less supervision.
But then he hit a plateau.
Leah credits John’s therapists with helping him slowly accept where he was at while continuing to push him in ways that led to more gradual improvement. In late December 2019, John wrapped up outpatient physical and occupational therapies. He’d continue speech therapy for a bit longer.
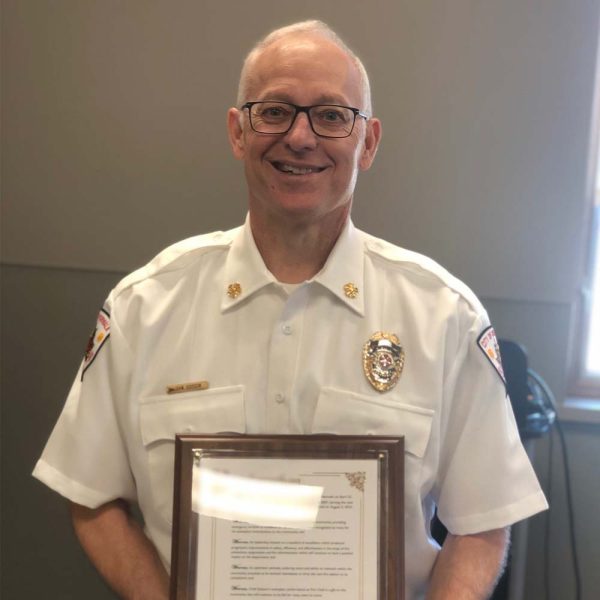
After nine months away from the Norwalk Fire Department, John returned for one last symbolic eight-hour shift on March 13, 2020. Then he retired, ending a 28-year career.
That summer, John started bike riding and golfing again. Today, he plays golf twice a week with friends and in a league where he’s the youngest player by 20 years. He’s active in local stroke support groups, has been a featured speaker at local events and is on the board of the Huron County Board of Mental Health and Addiction Services.
He takes medications to manage anxiety, to boost his concentration and energy, and to prevent seizures. He still tires easily. He no longer drives.
All this John shared in June 2024 when he and Jeanne met with Agnieszka A. Ardelt, MD, PhD, Chair, Department of Neurology and Director of Stroke Programs at MetroHealth. She oversaw John’s care in the NCCU.
It was the first time all three had been in the same room since John’s five days in the NCCU.
The Soissons thanked her for John’s lifesaving care. She quickly emphasized the collaborative culture that started at Fisher-Titus and continued in the NCCU.
“Many people interacted with him along his journey, not only there but also in acute rehab,” Dr. Ardelt said before the meeting. That teamwork – at which she says MetroHealth excels – extended to outpatient rehab, critical for the best outcome.
Dr. Ardelt reminded John that he’s a huge part of his ongoing recovery.
“We don’t control the hand that’s dealt us,” she told him. “What we do control is how we adapt to it. You’re a great role model and spokesperson.”
John says he has embraced being that spokesperson.
“Before all of this, I always pushed having a positive attitude,” he said. “It’s a frustrating disease, but I’ve got to look forward and improve every day.
“I want to make sure I continue to be that example.”
MetroHealth Rehabilitation Institute
Leaders in rehabilitation, research, and education to improve care for the most complex injuries and illnesses. Visit our website for more information about the MetroHealth Rehabilitation Institute or call:
- Outpatient appointments for adults and children, call 216-778-4414
- Inpatient services or admission for adults and children 13 yrs+, call 216-778-4167
Do you want to help patients like John? The MetroHealth Foundation is making a difference every day. Learn more or give at metrohealth.org/foundation.