Denise Janson’s amniotic sac began to leak when she was just 17 weeks pregnant. She and her husband decided MetroHealth’s Prematurity Clinic was the best chance for their unborn child.
It was love at first sight for Denise and Mike Janson. They met on the job as police officers in a Cleveland suburb. They had been dating for four years when Denise found out she was pregnant in 2008. Because they had been told that Denise would be unable to conceive, they were in a bit of happy shock when they got the news. They married on Oct. 25, 2008.
Denise’s amniotic sac (the membrane lining inside the uterus that contains the fetus) began to leak when she was just 17 weeks pregnant. She was diagnosed with Preterm Premature Rupture of the Membrane (PPROM), a rare condition that is usually deadly for the fetus. An obstetrics specialist told Denise she would likely miscarry and was counseled on the option of ending her pregnancy.
“We immediately looked on the Internet to see what my problem was and who could fix this,” she recalls.
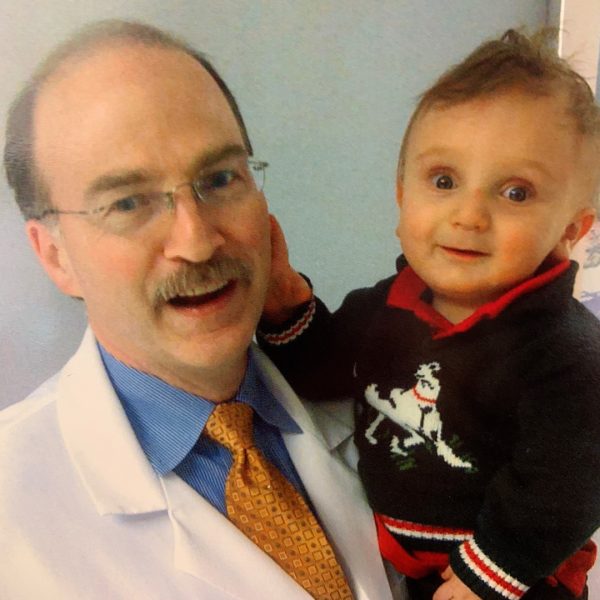
They found specialists at MetroHealth who could help. Soon after, they met with Brian Mercer, MD, Director of the Division of Maternal-Fetal Medicine and Obstetrics and an expert in PPROM.
After a day of tests, the Janson’s returned the following week and found some hope. Marc Collin, MD, a neonatologist, told them that if Denise could make it to 23 weeks, then there was a chance—with MetroHealth’s expertise—that she would be able to deliver a viable baby.
Back in 2009, the survival of a baby born at 23 weeks was in the 25-35% range, with more than half of babies having severe disabilities. Since then, the survival rate has risen to more than 50%.
Denise and Mike Janson decided MetroHealth’s Prematurity Clinic was the best chance for their unborn child. The Prematurity Clinic prepares a baby to be in the most optimal condition possible if preterm birth is inevitable. So two days before Christmas, Denise was admitted.
Denise’s room became a hub for nurses, who often took their lunch breaks with her.
“We were literally watching her belly grow,” recalls Annmarie Gorman, RN. “She was just incredible—always positive, with a huge, huge faith.”
During that time, Dr. Mercer was using an antibiotic regimen that he developed to help Denise’s baby survive. The regimen consists of administering ampicillin and erythromycin intravenously every six hours for 48 hours. This is followed by an oral dose of amoxicillin and erythromycin every eight hours for five days.
A few hours before Denise was induced, Dr. Collin joked that he needed her to go into labor right at 3 p.m. the next day because there was a meeting he didn’t want to attend. “We all laughed,” she says. “But at 3:05 p.m. the next day, they started paging everyone. Matt was born at 3:14 p.m.”
Matthew Janson was born March 6, 2009, weighing 4 pounds, 5 ounces and 16 inches long. Denise delivered Matthew at 34 weeks of pregnancy.
The Jansons worried that Matthew would be born with underdeveloped lungs. They thought their fears were coming true when he emerged without a sound—the umbilical cord had wrapped around his neck.
But after a few moments, one of the NICU doctors brought Matthew over to the couple. He was going to be OK. Matthew was then whisked off to the NICU, where he stayed for 10 days.
“I remember loading up the car at the hospital thinking, ‘We’re going home,’” Denise says. “After all that we had been through, I was so worried about driving home.”
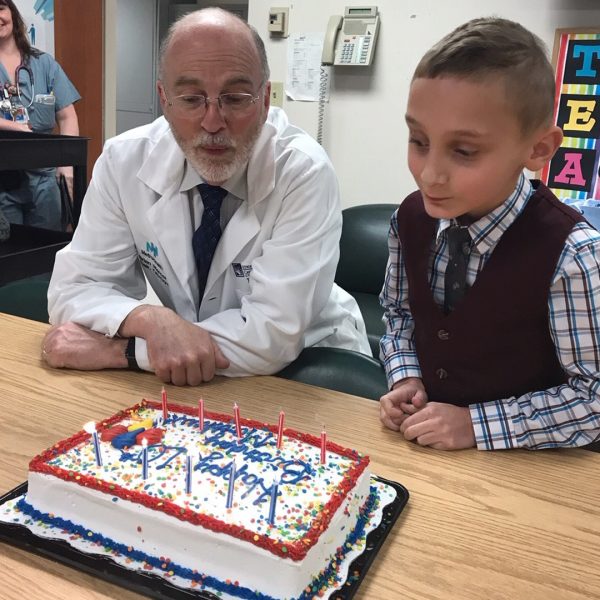
Today, Matt is in the 7th grade and recently celebrated his 13th birthday. Even though he has some gross motor skill delay with balance and is still a bit small for his age, he excels in school, was in Cub Scouts, and has already earned his black belt in kid’s karate.