Because of a kidney disorder she developed as a child, Meaghan Musarra always feared the medication used to treat her condition could prevent her from being able to have children.
Those fears were cast aside when she found out that she was pregnant with Addie.
The pregnancy was uneventful until Meaghan was diagnosed with severe preeclampsia, a sudden onset of high blood pressure during the third trimester of pregnancy that can affect the heart and other organs. Left untreated, the condition can cause serious health problems for a woman and her unborn baby.
Because of the preeclampsia, Meaghan’s labor was induced at 36 weeks. Addie arrived in September 2017, weighing 5 lbs. 1 oz, while mom and baby were able to go home after just one extra night in the hospital.
There was no question that the couple’s second baby, due in September 2019, would also be born at MetroHealth, but they had no way of knowing how different those two experiences would be.
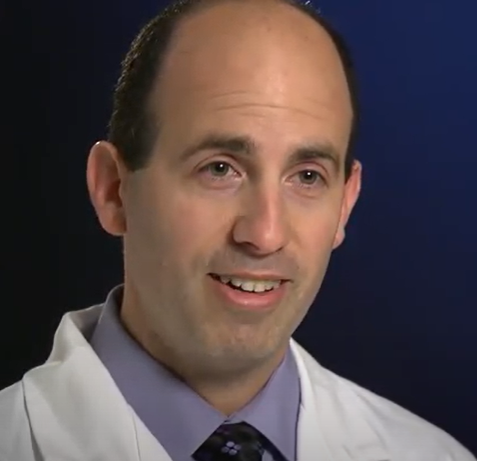
Meaghan’s kidney history and preeclampsia diagnoses with Addie deemed her second pregnancy high risk. She was referred to Bradley Stetzer, DO, a maternal-fetal medicine specialist, who focuses on high-risk pregnancies.
At 20 weeks, the goal was to monitor her more closely, with weekly imaging, tests and daily home blood pressure checks.
Dr. Stetzer’s first-hand experience of being a parent of an extremely premature baby, also born at MetroHealth, resonates with his patients.
“No doubt that experience has influenced not just what I do but part of me as a person,” he says.
On July 28, 2019, Meaghan’s at-home blood pressure read 150/110 and reached 190/115 upon arrival to The Labor and Delivery unit. Once again, she was experiencing severe preeclampsia. At 33 weeks pregnant, she was admitted and for three days received steroids to assist with fetal lung development and to reduce potential complications.
Dana Marcus, a Labor and Delivery nurse was part of her care team once again. Dana considers MetroHealth family as many of her relatives have worked there and she appreciates her team.
“We see the worst of the worst and the best of the best,” she says.
Dana was by Meaghan’s side on July 31 during induction. As the Musarras prepared for the NICU, Dana reassured them the NICU team would provide the best care.
After 38 hours, Dr. Stetzer delivered Magnolia (Maggie) on August 1, seven weeks early and 4 lbs. 10 oz.
After a few minutes of skin-to-skin contact, Maggie was taken to the NICU. Meaghan, under strict bed rest, wouldn’t see Maggie again for 24 hours.
MetroHealth’s NICU team spent the first few days stabilizing Maggie’s sugar and blood levels, treating her jaundice and monitoring her breathing. On Day 3 Meaghan and Brandon held their daughter, who was being fed intravenously and hooked up to monitors. The nurses also supported Meaghan’s desire to breastfeed, helping pump milk at bedside.
“No matter what background you come from our nurses and doctors treat every patient exactly the same,” says Kristen Uhler, one of the NICU nurses who tended to Maggie. “We treat every parent with respect they deserve.”
While Dr. Stetzer monitored Meaghan’s health, Biju Thomas, MD, a pediatrician, focused on Maggie. She needed help with feeding, a result of gestational age and medication given to Meaghan to treat preeclampsia.
On Day 7, Maggie’s IVs and tubes were removed. She could finally wear the preemie-sized onesies that were still too big on her.
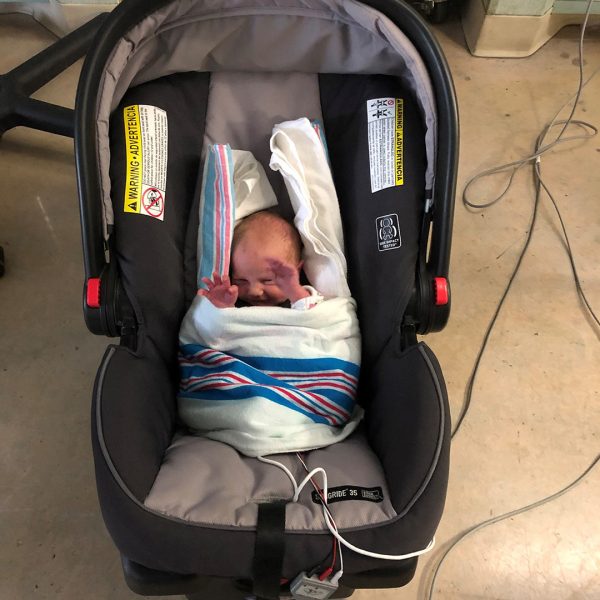
On Day 14, Maggie went home. At just over 5 lbs., she was smaller than one of her sister’s dolls.
Because of the early assistance from the NICU nurses, Meaghan fed bottled breast milk to Maggie for five months until she transitioned to nursing.
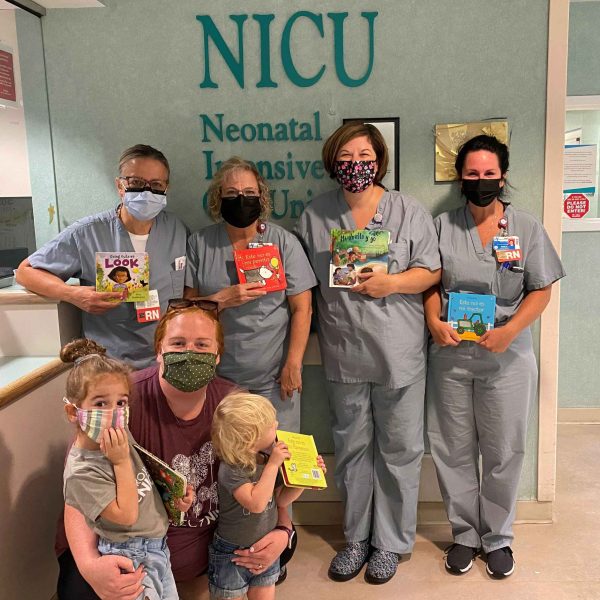
For two years, the Musarra family has supported Project NICU, a nonprofit that supports families with children in the NICU and the medical professionals who care for them. Meaghan is an ambassador for Project NICU, which supplies care packages for NICU families. In February 2021, the organization established the Project NICU Family Assistance Fund at MetroHealth to help families experiencing financial hardships while in the NICU.
To mark Maggie’s third birthday this year, the family raised $2,000 to purchase car seats for NICU families in need. A 2021 online fundraiser, in partnership with Usborne Books to purchase books for MetroHealth’s NICU library, raised more than $2,600. Books will be available in each of the private NICU rooms of the new Glick Center.
Diagnosed with hypotonia (low muscle tone), Maggie has received physical and occupational therapy since she was 9 months old. Her premature birth and hypotonia caused delays in activities like sitting up, standing and walking. Maggie took her first steps at 18 months.
Maggie wears ankle braces for added stability and muscle building, but they don’t slow her down. In February, Maggie took her first independent jump with both feet off the ground.
“She was born a fighter and is still a determined little girl,” Meaghan says. “She’s always happy.”
The past couple of months have kept the Musarras busy.
- Addie, 5, started Pre-Kindergarten.
- Maggie, 3, enrolled in preschool. She continues to go to physical and occupational therapy to improve her muscle tone.
- And on October 7, baby James Musarra was born, weighing 6 lb. 9 oz.
Once again, Dr. Stetzer had closely monitored Meaghan with the goal of avoiding a preeclampsia onset as long as possible.
This time, they avoided it altogether.
Dr. Stetzer induced Meaghan’s labor at 37 weeks – the standard of care for a woman with her health history.
And the Musarras all went home together.
Helping to manage the Musarras’ anxiety and worry during her pregnancy was no small feat, Meaghan says. “Dr. Stetzer is one of the calmest people I know. He had the ability to keep us on pace and to keep everything very grounded.
“Having him in our corner has been the reason we felt confident enough to continue our family.”