As a PhD student at Case Western Reserve University (CWRU), Kevin Kilgore, PhD, was intrigued by the use of technology to restore bodily movements and functions. Before long, he was named to the research team of Hunter Peckham, PhD. The opportunity marked the beginning of a decades-long collaboration to build a system that could adapt to both evolving technology and patient needs.
 Dr. Kilgore—now a staff scientist in the MetroHealth Center for Rehabilitation Research and the Departments of Physical Medicine and Rehabilitation (PM&R) and Orthopaedics—is helping carry on one of Dr. Peckham’s legacy projects after Dr. Peckham’s retirement: the Networked Neuroprosthesis, or NNP.
Dr. Kilgore—now a staff scientist in the MetroHealth Center for Rehabilitation Research and the Departments of Physical Medicine and Rehabilitation (PM&R) and Orthopaedics—is helping carry on one of Dr. Peckham’s legacy projects after Dr. Peckham’s retirement: the Networked Neuroprosthesis, or NNP.
The NNP has a natural home at the MetroHealth Rehabilitation Institute, which is world-renowned for Functional Electrical Stimulation (FES) research. Work on implantable FES systems began at the Institute in the 1980s. Dr. Peckham worked to develop a neuroprosthetic system that enabled individuals with spinal cord injury (SCI) to perform various functional activities of daily living, including eating, personal grooming and more.
The Beginning of No More Beginnings
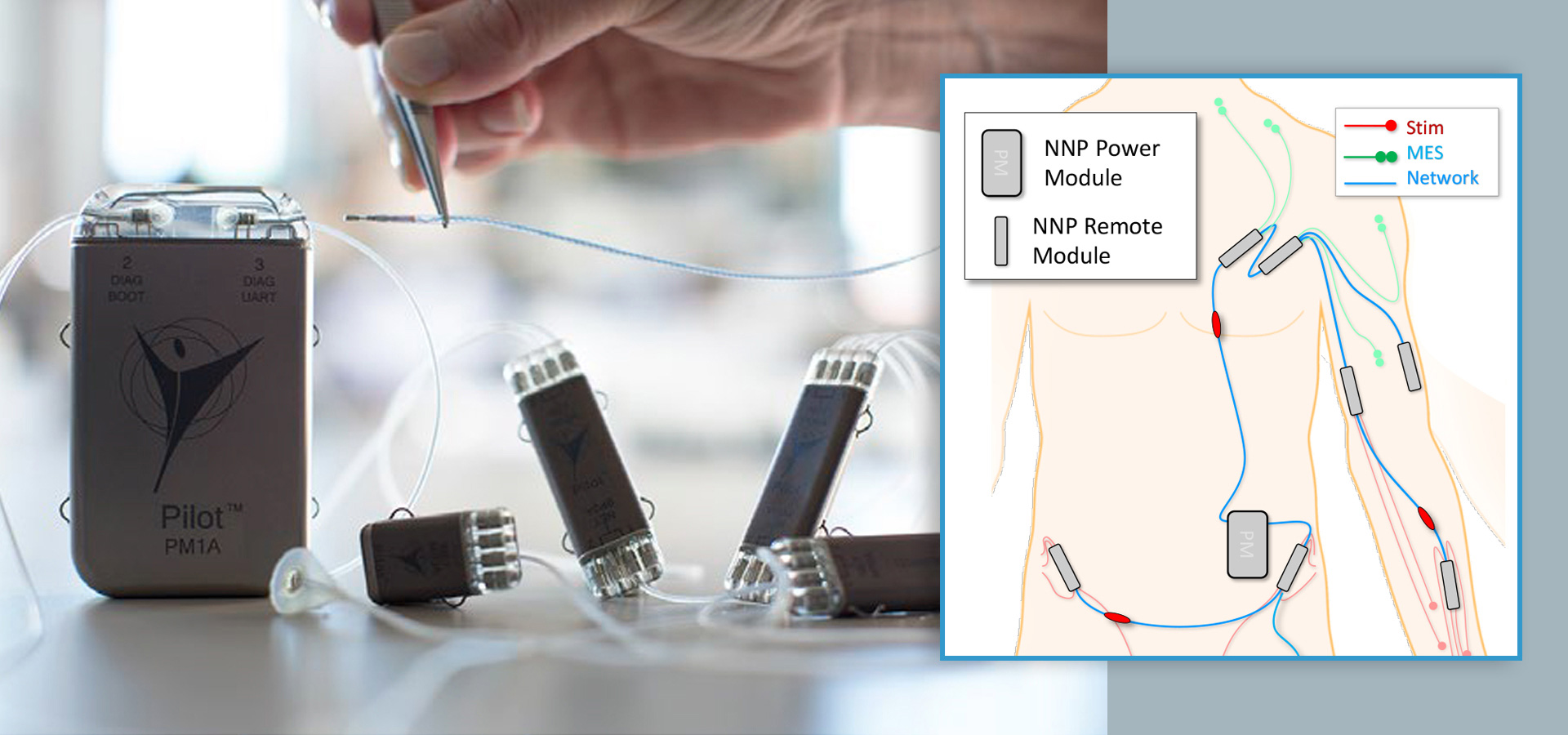
As technology evolved, so did the vision of what a neuroprosthetic system could do. Dr. Peckham and his team sought to expand the functions beyond hand movement to activities like improved posture, wheelchair propulsion and even bladder function. During this phase of designing, fabricating, implanting and implementing each new system iteration, the researchers proposed the idea of a modular implant concept.
“The modular idea came out of a conversation over breakfast in the late 1990s,” Dr. Kilgore recalls. “We were talking about what the future of implantable devices looked like—what would take it to the next level. We scribbled out our ideas for the modular concept on a napkin.”
Dr. Kilgore says the team didn’t want to design from the ground up each time they tried to evolve the technology in the neuroprosthetic system.
“The current design-and-redesign approach was inefficient. We needed a system we could modify without starting completely over,” he explains. “From there, the modular system was born. Most simplistically, think of NNP as a Lego kit for implantable devices.”
The modular concept gained traction after the research team secured a grant a few years after that pivotal breakfast meeting. In 2016, the NNP system was successfully implanted in humans for the first time.
A One-of-a-Kind Device
Dr. Kilgore explains that NNP is a network of modules inside the body, covering different locations depending on the targeted area and function. As a fully implantable system, the NNP is wired and capable of internal powering, processing and closed-loop control without requiring external components—except for battery recharge. When a new battery is needed, only one access point in the system needs to be reached, and this can be accomplished through a simple surgical procedure.
“There isn’t another modular system like this out therefor people with a spinal cord injury,” Dr. Kilgore says.
To date, the NNP has been implanted in nine participants in the arm, leg or trunk area—and in five of those participants, it’s in both their arm and trunk.
 Jeanette Green is one of the dual implant recipients. Thirty years ago, Jeanette suffered an SCI and received an implantable device to restore hand function in one of her hands. The device was one of the research team’s first-generation device inventions. (More about Jeanette)
Jeanette Green is one of the dual implant recipients. Thirty years ago, Jeanette suffered an SCI and received an implantable device to restore hand function in one of her hands. The device was one of the research team’s first-generation device inventions. (More about Jeanette)
“Jeanette was the beginning and end,” says Dr. Kilgore. “She received our first device in 1994, and in 2018, she came back and we added the NNP to her second hand as well as her trunk area—the latter helping with sitting posture.”
Sharing is Caring—For Humanity
The NNP has been developed on an open-source platform in the hope that it will accelerate the development of FES implantable devices.
“We decided on this approach to make ideas and technology as accessible as possible to the research community. Our goal is to eliminate or reduce barriers that accompany human study of these types of devices,” says Dr. Kilgore. “We believe this will accelerate research—especially since we’ve already gone through the regulatory process to test it in humans.”
While the NNP is now being tested in people with cervical-level spinal cord injury, the team is preparing to initiate a multi-center clinical trial of the hand system. Additionally, they have applied for a grant to study the NNP with bladder function added to hand and trunk function.